The therapeutic use of Platelet-Rich Plasma (PRP) has been investigated for various meniscal pathologies, including:
- Enhancing recovery following partial meniscectomy
- Non-operative management of meniscal degeneration or degenerative tears
- Facilitating healing in complex meniscal repairs
This mini-review critically examines the current evidence regarding the efficacy of PRP in treating these conditions.
PRP for Improving Recovery Following Partial Meniscectomy
A recent trial investigated the role of Platelet-Rich Plasma (PRP) in reducing inflammation and enhancing joint homeostasis following arthroscopic meniscal surgery. The randomized controlled trial conducted by Lo Presti et al. compared the effects of partial meniscectomy followed by a single injection of Autologous Conditioned Plasma (ACP) with those of partial meniscectomy alone in a cohort of 90 patients. [1] Results indicated that while the PRP group experienced an earlier reduction in Visual Analogue Scale (VAS) pain scores, there were no significant differences between the groups regarding pain relief, functional outcomes, objective measures, or return to sports at the six-month follow-up. The authors concluded that a single postoperative injection of PRP did not substantially enhance patient recovery after arthroscopic partial meniscectomy.
Duru et al. compared the injection of Amniotic Umbilical Cord Tissue (AMUC) versus PRP in 113 patients undergoing arthroscopic partial meniscectomy. Both PRP and AMUC groups showed improved outcomes compared to controls, with AMUC demonstrating superior patient-reported outcomes and a reduced reoperation rate compared to conventional techniques or adjunctive use of PRP at one year. [2]
PRP for Meniscal Degeneration Without Tear
Di Matteo et al, reported on the outcomes of 12 patients with meniscal degeneration who underwent 3 ultrasound (US) guided intra and peri-meniscal ACP injections 2 weeks apart. There was one failure, while the remaining patients had improved IKDC and VAS pain scores. [3]
Özyalvaç et al followed 15 patients undergoing US guided intra-meniscal injections with MRI scans. They reported increased Lysholm scores and regression of MRI signal in 67% of the cases at 32 months.[4]
It appears that symptomatic improvement can be obtained in patients with painful meniscal degeneration at short term follow-up. The improvements in MRI signal are promising but need to be confirmed with studies involving larger numbers of patients.
PRP for the Non-operative Treatment of Degenerative Meniscus Tears
The disappointing outcomes of degenerative meniscal tears treated with partial meniscectomy have led to a search for non-operative alternatives. Intra-meniscal and/or intra-articular PRP injections have been used alone or in combination for symptomatic treatment with positive short-term outcomes.
Two recent systematic reviews analyzed the effectiveness of PRP on the treatment of degenerative meniscal tears. Gopinatth et al. analyzed 6 studies including 184 patients, in which only one study was Level 1. PRP was effective for pain relief in most of the studies. Partial healing of the tear was observed in 0-40% of the studies and return to sports was reported in 60 to 100% of the studies. Due to the variability of outcomes, a definitive conclusion on PRP’s effectiveness could not be established [5] Elphingstone et al., reviewed 10 studies involving 686 patients undergoing intra-articular, intra-meniscal or combined PRP treatment. Most studies reported pain relief up to one year, however the effectiveness declined over time. The MRI signal was unchanged in 70-30% of the cases with 40-60% of studies showing some healing/improvement. Lower rates of subsequent arthroscopy and longer arthroscopy free survival were reported in several studies compared to controls. The authors concluded that PRP appears to be a safe and efficacious treatment strategy for degenerative meniscal pathology. However, due to diverse periprocedural techniques, PRP injectate characteristics, and a lack of high-quality studies, additional trials are needed to provide greater a degree of confidence in PRP’s clinical impact on patients with meniscus tears. [6]
Current literature suggests that PRP might play a role in the symptomatic treatment of degenerative meniscus tears. Healing or improvement of the tear varies across studies, with some showing no radiological improvement at all. The heterogeneity of studies due to diverse preparation & delivery methods of PRP and post-operative regimens underscores the need for further high quality research.
PRP for Augmentation of Meniscal Repairs
Fibrin clot and microfracturing the notch area have long been used to improve healing of complex meniscal repairs, such as tears in the avascular zone of the meniscus, radial tears or horizontal degenerative tears (Figure 1).
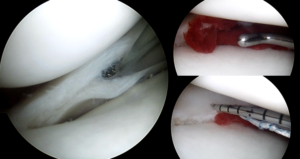 Figure 1 : Fibrin clot augmentation of the all inside repair of a horizontal degenerative cleavage tear of the medial meniscus.
Figure 1 : Fibrin clot augmentation of the all inside repair of a horizontal degenerative cleavage tear of the medial meniscus.
PRP has emerged as an adjunct to improve healing and decrease re-tear rates in these challenging cases. The utility of PRP has mostly been investigated for isolated meniscal tears, as the hemarthrosis in accompanying ACL tears is believed to have sufficient bioactive substances to promote a healing response. Furthermore, the addition of PRP has not been beneficial in these patients [7,8] . Early studies on PRP augmentation of meniscal tears showed promising results with decreased re-tear rates at 3 years for isolated meniscal tears [8] and improved healing rates for bucket handle tears. [9]
Since then, several meta-analyses have reported on the outcomes of PRP augmentation of meniscal repairs with conflicting conclusions. Belk et al., analyzed 6 comparative studies of 309 patients followed-up for 32 months. They could demonstrate no difference in failure rates (PRP 17% vs. control 22%) or in clinical outcomes. [10]
Li & Weng analyzed 9 studies (2 of them RCT’s) involving 1194 patients. The failure rate and VAS pain scores were significantly lower in the PRP group compared to controls (OR 0.64 & OR 0.76 respectively). [11] Xie et al., reviewed 8 randomized controlled trials including 431 patients. Compared to controls, patients receiving PRP had lower VAS pain scores and higher Lysholm scores, however, the healing rate was similar. [12] Migliorini et al, in their meta-analysis of 8 series involving 837 meniscal repairs, could not demonstrate a difference in VAS pain scores, Lysholm & IKDC scores, failures and revisions rates at 2-years follow-up between PRP and control groups. They concluded that the current published scientific evidence does not support PRP augmentation for arthroscopic meniscal repair. [13]
In a recent meta-analysis of RCT’s involving 139 meniscal repairs, Utrilla et al. showed a lower cumulative failure rate in patients augmented with PRP. None of the studies were able show improvement in MRI characteristics or clinical outcomes. [14] Finally a meta-analysis of 4 published meta-analysis of RCT’s showed a lower rate of failure of meniscal repairs with PRP augmentation. [15]
In conclusion, the beneficial effect of PRP on the repair of isolated & complex meniscal tears remains controversial. Given the absence of serious adverse events associated with PRP and the importance of saving the meniscus, every effort should be made to increase the healing rate of isolated complex and difficult-to-heal meniscal repairs, especially in younger patients. The emerging role of PRP and other orthobiologics will become clearer through studies involving larger number of patients and standardized PRP preparation, delivery methods and peri-operative regimens.
References
- Lo Presti M, Costa GG, Agrò G, Vasco C, Boffa A, Di Martino A, Andriolo L, Cenacchi A, Zaffagnini S, Filardo G. Platelet-Rich Plasma Injections Do Not Improve the Recovery After Arthroscopic Partial Meniscectomy: A Double-Blind Randomized Controlled Trial. Am J Sports Med. 2024 Nov;52(13):3198-3205.
- Duru N, Williams G Jr, Assid E, Renshaw A, Jones D. Comparative, Controlled, Retrospective Study of Patient-Reported Outcomes After Meniscectomy With Adjunctive Use of Platelet-Rich Plasma or Amniotic Umbilical Cord Tissue. Ochsner J. 2024 Spring;24(1):6-13.
- Di Matteo B, Altomare D, Garibaldi R, La Porta A, Manca A, Kon E. Ultrasound-Guided Meniscal Injection of Autologous Growth Factors: A Brief Report. Cartilage. 2021 Dec;13(1_suppl):387S-391S.
- Özyalvaç ON, Tüzüner T, Gürpinar T, Obut A, Acar B, Akman YE. Radiological and functional outcomes of ultrasound-guided PRP injections in intrasubstance meniscal degenerations. J Orthop Surg (Hong Kong). 2019 May-Aug;27(2):2309499019852779.
- Gopinatth V, Batra AK, Chahla J, Smith MV, Matava MJ, Brophy RH, Knapik DM. Degenerative Meniscus Tears Treated Nonoperatively With Platelet-Rich Plasma Yield Variable Clinical and Imaging Outcomes: A Systematic Review. Arthrosc Sports Med Rehabil. 2024 Feb 23;6(2):100916.
- Elphingstone JW, Alston ET, Colorado BS. Platelet-rich plasma for nonoperative management of degenerative meniscal tears: A systematic review. J Orthop. 2024 Mar 12;54:67-75.
- Bailey L, Weldon M, Kleihege J, Lauck K, Syed M, Mascarenhas R, Lowe WR. Platelet-Rich Plasma Augmentation of Meniscal Repair in the Setting of Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2021 Oct;49(12):3287-3292.
- Everhart JS, Cavendish PA, Eikenberry A, Magnussen RA, Kaeding CC, Flanigan DC. Platelet-Rich Plasma Reduces Failure Risk for Isolated Meniscal Repairs but Provides No Benefit for Meniscal Repairs With Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2019 Jul;47(8):1789-1796.
- Kaminski R, Kulinski K, Kozar-Kaminska K, Wielgus M, Langner M, Wasko MK, Kowalczewski J, Pomianowski S. A Prospective, Randomized, Double-Blind, Parallel-Group, Placebo-Controlled Study Evaluating Meniscal Healing, Clinical Outcomes, and Safety in Patients Undergoing Meniscal Repair of Unstable, Complete Vertical Meniscal Tears (Bucket Handle) Augmented with Platelet-Rich Plasma. Biomed Res Int. 2018 Mar 11;2018:9315815.
- Belk JW, Kraeutler MJ, Thon SG, Littlefield CP, Smith JH, McCarty EC. Augmentation of Meniscal Repair With Platelet-Rich Plasma: A Systematic Review of Comparative Studies. Orthop J Sports Med. 2020 Jun 17;8(6):2325967120926145.
- Li Z, Weng X. Platelet-rich plasma use in meniscus repair treatment: a systematic review and meta-analysis of clinical studies. J Orthop Surg Res. 2022 Oct 8;17(1):446.
- Xie YL, Jiang H, Wang S, Hu AL, Yang ZL, Mou Z, Wang Y, Wu Q. Effect of platelet-rich plasma on meniscus repair surgery: A meta-analysis of randomized controlled trials. Medicine (Baltimore). 2022 Aug 19;101(33):e30002.
- Migliorini F, Cuozzo F, Cipollaro L, Oliva F, Hildebrand F, Maffulli N. Platelet-rich plasma (PRP) augmentation does not result in more favourable outcomes in arthroscopic meniscal repair: a meta-analysis. J Orthop Traumatol. 2022 Feb 7;23(1):8.
- Utrilla GS, Degano IR, D’Ambrosi R. Efficacy of platelet-rich plasma in meniscal repair surgery: a systematic review of randomized controlled trials. J Orthop Traumatol. 2024 Dec 18;25(1):63.
- Sakti M, Paturusi IA, Singjie LC, Kusuma SA. The Use of Platelet-Rich Plasma Augmentation in Meniscus Repair Results in a Lower Failure Rate than in the Control Group: A Systematic Review From Meta-analysis. Arthrosc Sports Med Rehabil. 2024 Apr 9;6(4):100934.
Contact information:
Prof. Reha Tandogan, M.D.
Ortoklinik & Çankaya Orthopedics, Ankara, Türkiye
e-mail: rtandogan@ortoklinik.com